An Overview of Chlamydia and the Importance of Screening
- David Lee
- Sep 6, 2022
- 2 min read
More than 2.4 million cases of chlamydia, one of the most common sexually transmitted infections (STIs), were reported in the United States in 2020. However, this number likely underestimates the total number of infections as this STI often does not cause symptoms and routine healthcare services and STD screening were reduced during COVID-19.
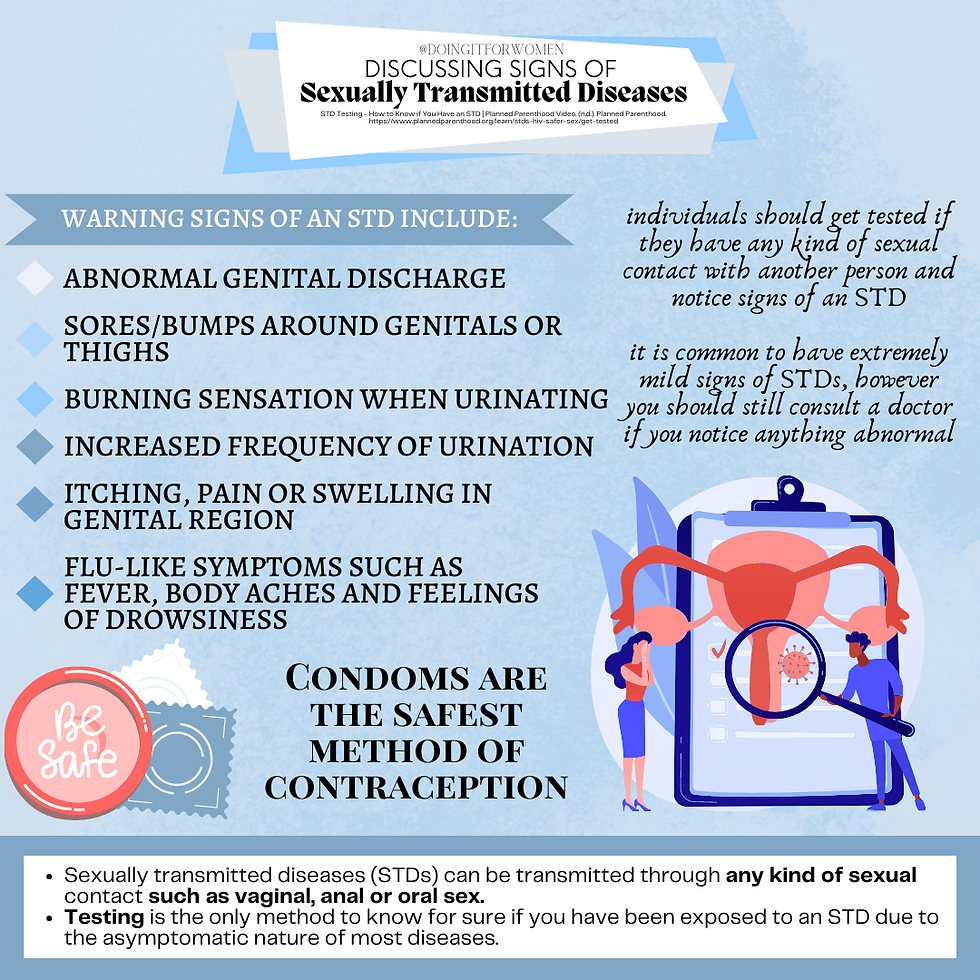
When symptoms do occur, the most commonly reported are pain while urinating, increased frequency of urination, and abnormal genital discharge. Since sexual practices have evolved over time, chlamydia infections are now seen in the mouth and anus as well. Common symptoms of an oral chlamydia infection include a sore throat that won’t go away, swollen lymph nodes and a low-grade fever, while common symptoms of anal chlamydia include rectal pain and itching.
Risk factors increasing the likelihood of a chlamydia infection include new sexual partners, having more than one sexual partner at a time, inconsistent condom use, and a history of a previous STI infection. Young people are disproportionately at risk for chlamydia, with most infections occurring between the ages of 15 to 24, and young women are at an even higher risk compared to young men. Most experts believe this is due to cervical ectopy (a benign gynecological condition), which causes the cervix of young women to be easily irritated during intercourse leaving them more susceptible to infection. Women are also at increased risk of long-term complications due to chlamydia, such as pelvic inflammatory disease (PID), ectopic pregnancy, and infertility.
Pelvic inflammatory disease, most commonly caused by chlamydia or gonorrhea, starts in the vagina or cervix and then spreads into the uterus, fallopian tubes, and sometimes the pelvic cavity. With proper treatment, most chlamydia and gonorrhea infections do not develop into PID; but for women who never show symptoms or who delay treatment, the long-term complications can be devastating. Studies show that a single PID infection can increase a woman’s rate of infertility by 8% (thought to be the result of fallopian tube scarring) and a second and third infection increases the infertility rate to 18% and 38%, respectively.
Screening programs for chlamydia and gonorrhea like urine samples and swabbing vaginal/cervical tissue during pelvic exams, reduce the number of women developing PID. Women who are uncomfortable with screening in a doctor’s office can purchase and use home-based kits. Current guidelines recommend that sexually active women under the age of 25 and women over the age of 25 who are at risk of STIs be screened once a year. In addition, pregnant women should be screened in the first trimester of pregnancy and again in the third trimester if they are at increased risk of STIs. Babies born to mothers with untreated chlamydia can develop complications such as preterm birth, low-birth-weight, neonatal conjunctivitis, and chlamydial pneumonitis.
Treatment of chlamydia with antibiotics is highly effective and, for this reason, the majority of resources should be focused on stopping transmission. The two best ways to accomplish this are by practicing safe sex through the use of condoms and increasing screening efforts across the country. Implementing screening guidelines for men, who can be infected and unknowingly transmit the infection to their sexual partners, could also decrease transmission rates.
References
Wiesenfeld H. C. (2017). Screening for Chlamydia trachomatis Infections in Women. The New England journal of medicine, 376(8), 765–773. https://doi.org/10.1056/NEJMcp1412935



Comments